
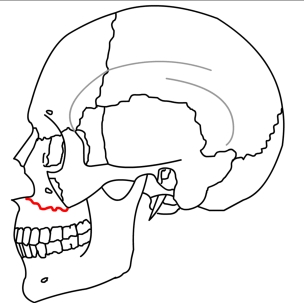
If a new missing tooth is identified, assess if the patient recalls coughing it out or swallowing it. Patient should be asked about new missing teeth or changes in the status of their teeth. Documentation of teeth is important, specifically the presence vs absence, condition (intact vs fractured vs decayed), mobility, and sensation. The presence of mucosal laceration overlying bony structures may suggest either alveolar or palatal fractures. Next, the oral cavity should be assessed for bleeding, mucosal lacerations, ecchymosis, and the presence of bone fragments or foreign bodies. If a LeFort II fracture is present, then both the nasal complex and the maxilla may move. If a LeFort I fracture is present, only the maxilla should move. Watch for movement in the maxilla and nasal complex. Assess the stability of the maxilla by firmly holding at the frontonasal suture with one hand and attempting manipulation of the anterior maxilla with the other hand. For the maxilla, bilateral external and internal palpation is often performed to assess for bony step-offs. If LeFort fractures are present, providers and/or patients may notice facial distortion, elongation or widening of structures, maxillary mobility, midface instability, and/or malocclusion.Ī systematic bony examination should be performed for all patients when concern for LeFort fractures. Pre-morbid photographs can be useful to assess symmetry and occlusion. Ecchymosis and edema may suggest underlying injury or facial fracture. Look for ecchymosis, edema, and facial lacerations. Removal of all dried blood, dirt, and dressings is important to have a comprehensive exam.įirst, inspect the patient's face and assess symmetry. The ability to review imaging prior to exam may guide additional attention to certain aspects. In the case of LeFort fractures, reduction of the maxilla and intermaxillary fixation (IMF) should decrease bleeding, but in some cases, angiographic embolization may be required.Ī thorough exam of the face is always warranted and documentation is critical. If present, ligation of cutaneous vessels and aggressive nasopharyngeal packing should be attempted to tamponade bleeding. Lastly, if there is concern for continued post traumatic hemorrhage and other well-known cavities for bleeding (abdomen, pelvis, thighs, chest) have been ruled out, then evaluation for hemorrhage from facial injury may be considered. Additionally, judicious use of oropharyngeal suctioning and minimal manipulation of the oral cavity is advised. Changes in the status of the airway can happen rapidly and having supplies for oral intubation and emergency airway management should be available. Such injuries will create difficult airway challenges, both in the ability to mask a patient and orally/nasally intubate. One-third of these patients will require discharge to a higher level of care facility than their location prior to injury.Īirway management is important after traumas involving the midface, due to bleeding, swelling, and changes in oral secretions management. Within the geriatric patient population, the ground level falls are a frequent source of facial fractures and may be indicative of functional decline. More attention to prevention of interpersonal violence may offer further reduction in the incidence of facial fractures. While integration of airbags and use of seatbelts in cars dramatically reduced facial fractures, In urban settings, most fractures were associated with interpersonal violence and MVAs, compared with in rural area, most fractures were associated with interpersonal violence, domestic accidents, work related accidents, and animal attacks. In a retrospective epidemiological study of midface fractures, the highest incidence was among patients aged 20–29 years old (35.9%), with a higher proportion among males (M:F, 9.6:1). A review of fifty-one articles on LeFort fractures showed that most are resultant from high-velocity MVA's and that the severity of fracture type sustained occurred with increasing frequency. Specifically, MVAs and gunshot wounds present commonly with a higher proportion of panfacial fractures, compared with sports-related accidents associated with upper midface fractures, and assaults that are linked to mandibular and nasal fractures. In the general population, the most common causes of facial fractures are associated with assaults and motor vehicle accidents (MVAs), 36% and 32%, respectively.Ī smaller percentage is accounted for by falls (18%), sport injuries (11%), occupational accidents (3%), and gunshot wounds (2%).Īdditionally, the mechanism of action of the injury can be associated with the presenting facial fracture pattern.


 0 kommentar(er)
0 kommentar(er)
